Dr. Timothy Sampson
"It is my belief that future discoveries in the field [of neurological disorders] will not solely rely on the study of the brain, but through the broad and multidisciplinary exploration of our microbial inhabitants."
I’m Timothy Sampson, and this is why I research.
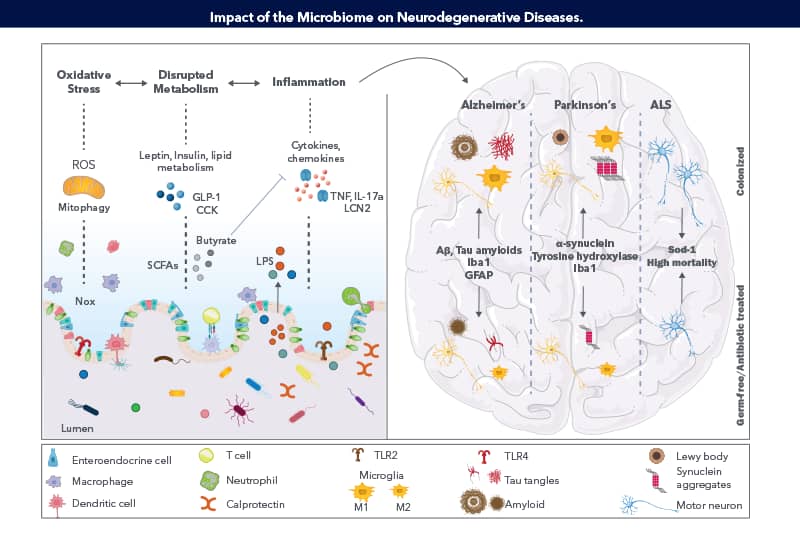
Dr. Timothy Sampson is Assistant Professor in the Department of Physiology at Emory School of Medicine. He trained as a postdoctoral fellow at Caltech in the laboratory of Dr. Sarkis Mazmanian, where he explored how indigenous microbes influence Parkinson’s disease (PD). His work identified that gut microbes are necessary for etiopathogenesis and that microbial communities derived from persons with PD significantly worsen motor dysfunction in a mouse model. Dr. Sampson’s research investigates host-microbe interactions at the interface of PD, Alzheimer’s disease (AD), and other neurological diseases historically studied within the context of the central nervous system. With his background in bacterial genetics and pathogenesis, coupled with growing excitement towards neuroscience, and a supportive, neurophysiology-focused academic department, Dr. Sampson’s research program is poised to address the inherently interdisciplinary questions within this emerging field. Similar to how the study of pathogens has informed the field of immunology, his work aims to reveal new pathways at the microbiota-brain interface.
Would you tell us about your career path and what first sparked your interest in science?
I have always had an interest in the living, microscopic world around us. My parents were very supportive and encouraging in getting various science books from the library and gave me and my siblings the opportunity to explore our many interests and passions as kids. I really was interested in studying infectious disease, almost romanticizing the emerging infectious disease researchers studying Ebola, and the like. It was clear to me that I should pursue microbiology. During my undergraduate studies I was privileged to have been part of a bacteriophage research lab, headed by Dr. Graham Hatfull and Deborah Jacobs-Sera, that supported many undergraduates in learning not only hands-on microbiology techniques, but also what it meant to do true bench research (as opposed to pre-canned lab activities). The mentorship and excitement there propelled me, and many others, into academic microbiology careers.
Some of your recent research focuses on microbiome produced amyloids promoting alpha-synuclein pathophysiology in the gut and brain. Can you briefly expand on your findings and what got you interested in studying the gut-brain axis?
While I was sparked by the idea of infectious disease, during my early studies I came to realize that pathogens and disease were actually a rare outcome of our interactions with microbes. Our bodies are in constant contact with microbes on every environmentally exposed surface. While pathogenesis is rare, these interactions are constant and numerous. The community of bacteria, viruses, and fungi in the gut (the gut microbiome) is an immense reservoir for unique bacterial species, genes, and metabolites, and outnumber our own cells and genes. In thinking about this community, it has such immense genetic and metabolic potential as to be thought of as its own organ system. Therefore, it stands to reason that the gut microbiome can affect the brain. I wanted to use my background in bacterial genetics and microbiology to better understand how these organisms can alter neurological outcomes across health and disease.
What are the current or proposed strategies for modulating intestinal microbes?
To me, I am most intrigued by the idea of dietary and so-called “prebiotics”. These have potential to alter the composition of the existing microbiome, (as opposed to trying to add in new members, like probiotics). Dietary interventions can also increase the resiliency of the microbiome, preventing drastic changes from occurring in the face of specific perturbations. So, these have some potential for both therapeutic and preventative effects.
Research has made it clear that gut dysbiosis is directly linked to neurodegenerative diseases. In your opinion what are the major or most intriguing studies that have led to this finding?
To me, the ever-increasing number of studies that have independently validated discrete changes to the gut microbiome in individuals who have these particular diseases, like PD, is most intriguing. For PD, we are at the point where a consensus is being built, and disease-linked signatures in the microbiome are being identified. Principle Investigators (PIs), like Dr. Haydeh Payami out of U. Alabama-Birmingham, are taking what we’ve learned in the study of genetic associations and are applying those same sorts of rigorous techniques to microbiome compositions. Coupling these large datasets with unique experimental models, such as germ-free and gnotobiotic mice, allows us to directly test how these distinct microbiome compositions affect host physiology in model systems.
What developments in the gut-brain axis field are most exciting to you and how do you see the field changing and advancing in the next few years?
The decreasing cost of shotgun/metagenomic sequencing and analysis will be a huge benefit for the field. Most of us profile the microbiome using 16S rRNA sequencing, which can be somewhat limited in identifying the exact species present, let alone the strain. This makes it difficult to know what these compositions mean, since we do not know what genes are actually present. Different microbiome compositions may actually have functional redundancy in their genetic and metabolic output, and lead to similar effects, even if the 16S composition looks different. We’ll be able to more easily identify beneficial or pathogenic changes in specific gene networks or metabolic products that are associated with and/or contribute to host physiology.
Tell us about what exciting research projects are happening in your lab.
We have a few primary research directions in the lab right now. In continuing the discussion on microbiome compositions, we are interested in understanding why certain neurodegenerative diseases, like PD, have altered microbiome compositions in the first place. The so-called chicken and egg problem. We are investigating whether external insults like chemical exposure, certain diets, and infections, that are associated with PD, can trigger a PD-like microbiome composition.
In addition, we are interested in identifying how certain signals from the gut microbiome can make their way to the brain. We are working to examine a link between certain gut-resident cells and the brain that may be a physical pathway for bacterial molecules to reach the brain.
Finally, we have also become extremely interested in how the microbiome changes after traumatic neurological injury. Since we know that microbiome changes can influence inflammatory responses, and chronic inflammation can be detrimental to injury recovery, we are working to identify specific beneficial microbes that may expediate recovery or limit co-morbidities after an injury.
What has been a successful guiding principle for mentoring in your lab?
I have always had mentors who were always available to me. Even if they did not have a direct answer, they were consistently a sounding board to talk through technical problems, scientific difficulties, and life events. I hope to cultivate that same open-door policy with all my mentees, and transparently share with them both the immense fun and the challenges that come with an academic track.
Do you have any advice for young scientists interested in pursuing a research career?
Try to take advantage of every research opportunity that interests you as early as possible. Don’t be afraid to reach out to PIs you are interested in working with, even if there is no job positing, or you don’t know them. Apply for every scholarship and award that comes your way. Be persistent and read everything you can.
What advice would you give to your young self about your path in science?
Don’t be shy and don’t be afraid to speak up. Be meticulous in your organization and planning.
And finally, COVID-19 has been a global challenge, requiring us to make many adjustments to our daily lives. What changes from the pandemic will you keep?
We are all certainly growing tired of Zoom meetings. However, I think this has made us realize that virtual conferences and meetings are not too difficult, still very useful, and can be especially beneficial when participants are located very far apart. I anticipate that certain seminars or even my occasional joint lab meeting with collaborators will maintain some virtual / teleworking aspect, even as in person lab meetings begin again.
Selected Publications
-
Challis, C., Hori, A., Sampson, T. et al. (2020) Gut-seeded α-synuclein fibrils promote gut dysfunction and brain pathology specifically in aged mice. Nature neuroscience
-
Sampson, T. R., Challis, C. et al. (2020) A gut bacterial amyloid promotes α-synuclein aggregation and motor impairment in mice. eLife
-
Sampson T. (2020) The impact of indigenous microbes on Parkinson's disease. Neurobiology of disease
-
Fields, C. T., Sampson, T. R. et al. (2018) Defining Dysbiosis in Disorders of Movement and Motivation The official journal of the Society for Neuroscience
-
Sharon, G., Sampson, T. R. et al. (2016) The Central Nervous System and the Gut Microbiome. Cell
-
Sampson, T. R., & Mazmanian, S. K. (2015) Control of brain development, function, and behavior by the microbiome. Cell host & microbe