By Jamshed Arslan, Pharm. D., PhD.
What Are GluTs?
Mammalian cell metabolism is incomplete without glucose. Glucose is a monosaccharide that is transported to the cells through facilitative diffusion, a process governed by membrane proteins like glucose transporters (GluTs).1 GluTs belong to a large family of membrane transporters, called Major Facilitator Superfamily (MFS), found in virtually all forms of life.1,2 Specifically, GluTs belong to the subfamily Sugar Porters whose members take part in the uptake of monosaccharides and disaccharides.1 Human glucose transporter GluT1 shuttles glucose to the organs with limited access to small molecules like glucose via passive diffusion.3
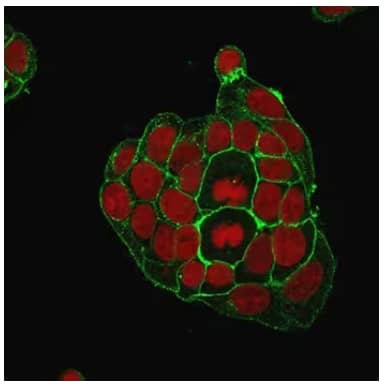
Immunofluorescence staining of breast cancer line MCF-7 cells using Mouse Monoclonal GluT1 Antibody (NBP2-75785) followed by goat anti-Mouse IgG conjugated to CF488 (green). Nuclei are stained with Red Dot.
GluT1 in health and disease
GluT1 mediates glucose uptake into red blood cells (RBCs) and endothelial cells of the blood-brain barrier (BBB).1 Although GluT1 is famous for glucose transport, it can also transport other small molecules like galactose, glucosamine, mannose and dehydro-L-ascorbic acid.1,4 Both higher and lower expressions of GluT1 are dangerous: many tumors overexpress GluT1 whereas GluT1 deficiency has been reported in several diseases of the central nervous system like psychomotor retardation and epilepsy.3,5
More than 250 cases of GluT1-deficiency syndrome (GDS) have been reported since the year 1991 when the GDS was first described.3 GDS occurs as a result of mutations in SLC2A1 gene that exhibits autosomal dominant inheritance.5 The lack of glucose transport in GDS, evidenced partly by glucose levels below 40 mg/dl in cerebrospinal fluid, is typically treated with ketogenic (high-fat) diet. Ketone bodies produced as a product of this diet can cross BBB to serve as an alternative fuel for the brain.3,5
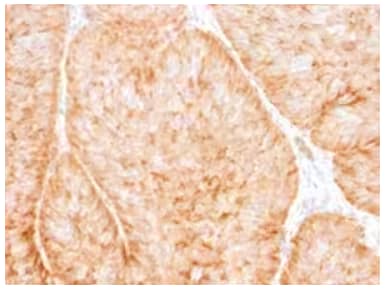
Immunohistochemistry analysis of formalin-fixed, paraffin-embedded human bladder carcinoma stained with GluT1 Mouse Monoclonal Antibody (NBP2-75784).
Highlights from current research on GluT1:
GluT1 is an intensively studied membrane transport protein. Its role in various cancers has been the focus of many research groups around the world.
- GluT1 as a drug target in glioblastoma multiforme: GluT1 and one of its binding partners, Tubulin 4, have been discovered as druggable targets in this deadliest brain tumor.6 Using human glioblastoma patient samples, the researchers in US and Canada found that GluT1 overexpression is linked to poor prognosis and inhibiting GluT1/Tubulin 4 significantly reduces cancer proliferation.6
- miRNA‑10a promotes oral cancer by upregulating GluT1: Scientists in China found that miRNA‑10a and GluT1 are overexpressed in oral squamous cell carcinoma (OSCC) patient samples relative to the adjacent healthy tissues.7 By knocking down GluT1 in OSCC cells, they showed that miRNA‑10a-mediated cell proliferation requires GluT1.7
- Overexpression of ChREBP with GluT1 is associated with liver cancer: A team of investigators in China and Netherlands studied the expression patterns of carbohydrate response element binding protein (ChREBP) and various GluTs in multiple stages of human hepatocellular carcinoma.8 They found that overexpression of ChREBP and GluT1, but a reduced expression of GluT2, was positively correlated with malignancy.8
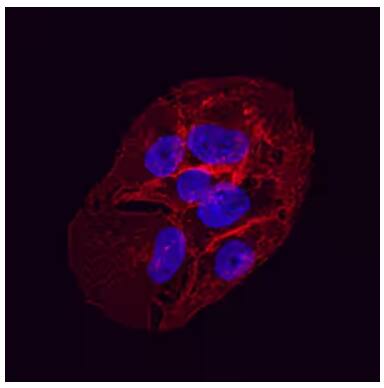
Immunocytochemistry/Immunofluorescence showing GluT1 detected in immersion fixed HepG2 human hepatocellular carcinoma cell line using Mouse Anti-Human Glut1 Monoclonal Antibody (MAB1418) at 10 µg/mL for 3 hours at room temperature. Cells were stained using the NorthernLights™ 557-conjugated Anti-Mouse IgG Secondary Antibody (red; NL007) and counterstained with DAPI (NBP2-31156) (blue). Specific staining was localized to the plasma membrane.

Jamshed Arslan, Pharm D, PhD
Dr Arslan is an Assistant Professor at Barrett Hodgson University, Pakistan,
where he uses various pedagogical methods to teach Pharm D students.
-
Galochkina, T. et al. (2019) New insights into GluT1 mechanics during glucose transfer Scientific Reports
-
Yeagle, PL. (2016) Membrane transport The Membranes of Cells (3rd ed)
-
Simmons, RA. (2017) Cell glucose transport and glucose handling during fetal and neonatal development. Fetal and Neonatal Physiology (5th ed)
-
Hosoya, K., Kubo, Y. (2014) Vitamin transport across the blood–retinal barrier: Focus on vitamins C, E, and biotin Handbook of Nutrition, Diet and the Eye
-
Leturque, A. et al. (2012) Carbohydrate intake Progress in Molecular Biology and Translational Science.
-
Guda, MR. et al. (2019) GLUT1 and TUBB4 in glioblastoma could be efficacious targets Cancers
-
Chen, Y. et al. (2019) miRNA‑10a promotes cancer cell proliferation in oral squamous cell carcinoma by upregulating GLUT1 and promoting glucose metabolism Oncology Letters
-
Lei, Y., Hu, Q., & Gu, J. (2019) Expressions of carbohydrate response element binding protein and glucose transporters in liver cancer and clinical significance Pathology & Oncology Research