By Victoria Osinski, PhD
As our daily routines shift away from those of the peak pandemic days in 2020 and 2021, you may have found yourself or others getting sick a little more often this fall and winter. In November 2022, The Centers for Disease Control (CDC) Health Alert Network released a health advisory reporting increased respiratory virus activity. The frequency of infections and hospitalizations, especially amongst children, were higher than years prior and the CDC found increased incidence of both respiratory syncytial virus (RSV) and influenza viruses.1 The CDC reports that hospitalizations due to RSV peaked earlier and at a higher frequency than in the past four winter seasons.2 Fortunately, influenza hospitalization frequency and percentage of outpatient visits did not surpass that of prior years but did, like RSV, peaked earlier in the season.3 As we observe these earlier infections, it may be helpful to discuss what exactly these viruses are, how we get sick from them, and what happens when someone is infected with both viruses simultaneously.
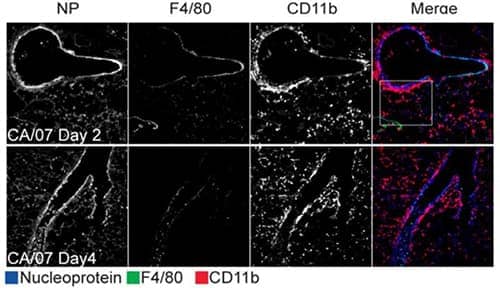
Immunohistochemical analysis showing Influenza A virus (A/California/07/2009(H1N1)) induced expression of nucleoprotein in frozen lung tissue sections of airway epithelial cells collected two- and four-days post-infection. Sections were probed for Rabbit anti-Influenza A H1N1 Nucleoprotein Polyclonal Antibody (Catalog # NB100-56570) (blue), anti-F4/80 antigen (green), and anti-CD11b (red). Staining revealed substantial recruitment of CD11b+ cells while F4/80+ cells were minimally detected. Image collected and cropped by CiteAb from the following publication (//dx.plos.org/10.1371/journal.pone.0076708) licensed under a CC-BY license.
Influenza and RSV: Virus Definitions, Spread, and Symptoms
Influenza
First, let’s clarify some terminology: Influenza, commonly called the flu, is the respiratory illness that is experienced due to infection by influenza viruses. There are four types of influenza viruses: Influenza A, -B, -C, and -D.4 These viruses contain segmented, negative-strand RNA genomes, which encode all the proteins needed to form new viral particles. In a complete viral particle, the RNA is surrounded by a membrane that contains specific types of proteins termed glycoproteins. The specific glycoproteins on influenza viruses are called hemagglutinin (H) and neuraminidase (N).4,5 There are many subtypes of H and N, which are used to characterize and name the many different strains of influenza that have evolved over the years. Check out more information about influenza virus nomenclature on the CDC pages. Influenza viruses survive in liquid droplets and at lower temperatures and are spread when infected individuals cough, sneeze, or talk. To spread the virus, liquid droplets may either contact another individual’s mouth or nose or may land on surfaces that others touch.6 To infect a person, the virus must enter the respiratory tract where particles can attach to and enter cells and replicate. Since this virus infects the respiratory system, common symptoms of the flu include cough, sore throat, and a runny or stuffy nose. Often, infected individuals will also experience fever, aches, and fatigue due to the anti-viral immune response.6
RSV
Like Influenza viruses, RSV consists of a single, negative-stranded RNA that is encapsulated by a membrane containing glycoproteins. These glycoproteins called attachment (G) and fusion (F) proteins are important for viral particles’ attachment to and entrance into cells. It is understood that RSV infection is restricted to specific cell types within the lung and airway: ciliated airway epithelial cells and type I alveolar pneumocytes.7 Like the flu, RSV-infected individuals will often experience a runny nose, cough, sneezing, and a fever. Other common symptoms include wheezing and a decrease in appetite.8
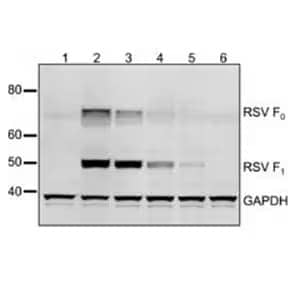
Western Blot analysis showing RSV expression in the lysates of cells infected with (1) vector without Fusion (F) protein gene, (2 to 5) a vector containing the F gene at various positions, and (6) mock transfected, then probed with Mouse anti-Respiratory Syncytial Virus Monoclonal Antibody (2F7) (Catalog # NB110-37246). GADPH was used as a loading control.
Current Preventative Measures
To prevent spread of influenza and RSV, it is important to wash hands often, cover one’s mouth and nose with coughing and sneezing, and avoid close contact with those that are already sick. Additionally, yearly influenza vaccines are produced and administered in the fall as “flu season” begins. The flu vaccine helps prime the immune system to produce antibodies that recognize and aid in eliminating the virus (ideally) before causing too many symptoms. Unfortunately, a vaccine for RSV is not yet available*, but palivizumab, a monoclonal antibody injection, is an option for high-risk infected individuals (infants and children) to prevent severe illness.8
Influenza and RSV: A Potential for More Severe Illness When Combined?
At times, individuals may be infected with RSV and influenza viruses concurrently and a few studies estimate that about 10 to 30% of respiratory illnesses in children are due to these co-infections.9,10 To study how co-infection may influence viral interactions and infection outcomes, a group from the University of Glasgow in Scotland infected epithelium cell cultures with both viruses and characterized resultant viral particle glycoproteins and attachment features using advanced imaging techniques.11 Interestingly, they found that many cells were infected with both types of viruses during co-infection and further identified hybrid viral particles that contained glycoproteins from both viruses. These hybrid particles were able to infect primary bronchial epithelium cells and facilitated viral entry into epithelial cell lines that were modified to prevent entry by influenza viral particles alone. This study demonstrates that co-infection of individual airway cells with both viruses is biologically feasible and speculate that this could aid in antibody evasion. Further studies will be needed to translate these findings into a true upper respiratory infection setting. If they do translate, future efforts will have to focus on developing improved vaccination and treatment approaches to prevent more severe disease in co-infected individuals.
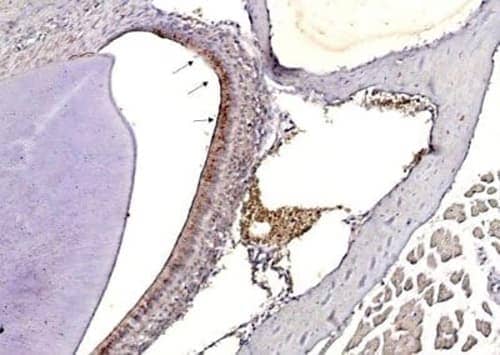
Immunohistochemical detection of Influenza A H3N2 Hemagglutinin (HA) protein in paraffin-embedded mouse nasal tissue infected with Influenza Virus A using Rabbit anti-Influenza A H3N2 HA Polyclonal Antibody (A/Taiwan/3446/02) (Catalog # NBP3-12877).

Victoria (Tori) Osinski, PhD
University of Minnesota Medical School
Victoria is doing her post-doctoral research fellowship at the Center for Immmunology studying vascular and immune mechanisms driving autoantibody-mediated mitral valve disease.
*Update November 2024: There is now a FDA-approved vaccine available for older adults12,13.
-
CDC Health Alert Network (2022) Increased Respiratory Virus Activity, Especially Among Children, Early in the 2022-2023 Fall and Winter. Centre for Disease Control and Prevention
-
Centers for Disease Control and Pre (2022) RSV-NET: Respiratory Syncytial Virus Hospitalization Surveillance Network, Centers for Disease Control and Prevention.
-
Centers for Disease Control and Pre (2023) Weekly U.S. Influenza Surveillance Report.
-
Centers for Disease Control and Pre (2022) Types of Influenza Viruses.
-
Bouvier NM, Palese P. (2008) The biology of influenza viruses. Vaccine 26:D49-53.
-
Centers for Disease Control and Pre (2022) Key Facts About Influenza (Flu).
-
Battles MB, McLellan JS. (2019) Respiratory syncytial virus entry and how to block it. Nat Rev Microbiol. 17:233-245.
-
Centers for Disease Control and Pre (2022) Respiratory Syncytial Virus Infection (RSV).
-
Nickbakhsh S, Thorburn F, et al. (2016) Extensive multiplex PCR diagnostics reveal new insights into the epidemiology of viral respiratory infections. Epidemiol Infect. 144:2064-2076.
-
Franz A, Adams O, Willems R, et al. (2010) Correlation of viral load of respiratory pathogens and co-infections with disease severity in children hospitalized for lower respiratory tract infection. J Clin Virol. 48:239-245.
-
Haney J, Vijayakrishnan S, et al. (2022) Coinfection by influenza A virus and respiratory syncytial virus produces hybrid virus particles. Nat Microbiol. 7:1879.
-
GSK Press Release (2023) GSK announces AREXVY, its respiratory syncytial virus (RSV) vaccine, is now available at all major US retail pharmacies
-
Pfizer Press Release (2023) U.S. FDA Approves ABRYSVO™, Pfizer’s Vaccine for the Prevention of Respiratory Syncytial Virus (RSV) in Older Adults