Analysis of Cetuximab by Maurice
Introduction
Cetuximab targets the epidermal growth factor receptor (EGFR). It is used as a therapeutic agent in the treatment of a number of cancers including colorectal, head and neck cancer1,2. Cetuximab was approved by the FDA in 2004, and its US patent expired in 2016.
Maurice icIEF Method
Carboxypeptidase B (CpB) treatment: Cetuximab was diluted to 1.0 mg/mL in water prior to CpB digestion. CpB (1 mg/mL stock solution) was added at a ratio of 1:100 (CpB to sample) and incubated at 37 °C for 20 minutes and then placed on ice. CpB was obtained from Sigma-Aldrich (PN C9584).
Sample preparation: Cetuximab was diluted to 0.2 mg/mL in the ampholyte solution.
Ampholyte solution: Pharmalytes 8–10.5 (3%) and 5–8 (1%) containing 3.2 M urea, 5 mM IDA and10 mM arginine.
pI markers: 5.85 and 10.17.
Running conditions: 1 minute at 1500 V, then 8 minutes at 3000 V.
Imaging: Absorbance and fluorescence. Recombinant: The cetuximab biosimilar was obtained from R&D Systems, PN MAB9577.
Results
To compare cetuximab to a recombinant, we used the icIEF platform method described above to monitor charge heterogeneity by absorbance (Figure 1) and by native fluorescence detection (Figure 2). These analyses revealed noteworthy differences between the molecules. For example, the innovator has two peaks in the basic region that disappear upon treatment with CpB (Figure 1, 2), suggesting that the innovator has terminal-lysine containing variants that are absent in the recombinant.

Figure 1. icIEF absorbance (top) and peak area percentages (bottom) of cetuximab and a recombinant.
| Sample | Acidic Region | Main Peak | Basic Region | Δ Basic Region | |
|---|---|---|---|---|---|
|
Cetuximab |
No treatment | 54.3 | 28.6 | 17.1 | N/A |
| CpB-treated | 70.0 | 30.0 | 0.0 | -17.1 | |
|
Recombinant |
No treatment | 81.4 | 16.9 | 1.7 | N/A |
| CpB-treated | 81.8 | 17.0 | 1.3 | -0.4 | |
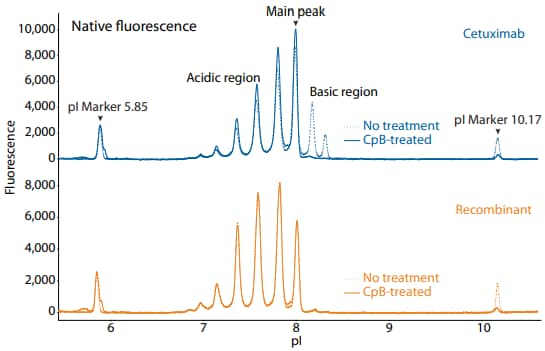
Figure 2. icIEF fluorescence (top) and peak area percentages (bottom) of cetuximab and a recombinant.
| Sample | Acidic Region | Main Peak | Basic Region | Δ Basic Region | |
|---|---|---|---|---|---|
|
Cetuximab |
No treatment | 56.2 | 27.7 | 16.1 | N/A |
| CpB-treated | 70.7 | 28.2 | 1.1 | -15.0 | |
|
Recombinant |
No treatment | 83.6 | 15.7 | 0.7 | N/A |
| CpB-treated | 83.0 | 16.5 | 0.5 | -0.2-0.4 | |
Maurice CE-SDS Method
Sample preparation: Cetuximab was diluted to 1 mg/mL with 1X Sample Buffer prior to treatment for 10 minutes at 70 °C in the presence of either 11.5 mM IAM (nonreducing) or 650 nM β-ME (reducing).
Running conditions: Samples were injected for 20 seconds at 4600 V, followed by a 25-minute separation (reducing) or a 35-minute separation (non-reducing) at 5750 V.
Results
Cetuximab and a recombinant were analyzed on the CESDS platform method described above under reducing (Figure 3) and non-reducing (Figure 4) conditions. These analyses revealed differences in peak area percentages, for example the heavy chain under reducing conditions and the intact mAb under non-reducing conditions.
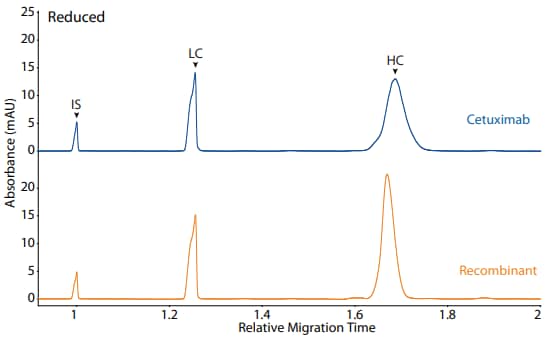
Figure 3. CE-SDS reduced (top) and peak area percentages (bottom) of cetuximab and a recombinant. (IS) Internal standard. (LC) Light chain. (NGHC) Non-glycosylated heavy chain. (HC) Heavy chain.
| Sample | Other | NG | Intact |
|---|---|---|---|
| Cetuximab | 1.5 | 4.0 | 94.5 |
| Recombinant | 3.5 | 7.7 | 88.7 |

Figure 4. CE-SDS non-reduced (top) and peak area percentages (bottom) of cetuximab and a recombinant. (IS) Internal standard. (NG) Non-glycosylated.
| Sample | LC | NGHC | HC | Other |
|---|---|---|---|---|
| Cetuximab | 30.0 | 0.2 | 69.4 | 0.3 |
| Recombinant | 30.1 | 0.9 | 67.7 | 1.3 |
References
- Cetuximab: from bench to bedside, B Vincenzi, A Zoccoli, F Pantano, O Venditti and S Galluzzo, Current Cancer Drug Targets, 2010; (10)1:80–95.
- New thearpies in head and neck cancer, R Santuray, D Johnson and J Grandis, Trends Cancer, 2019; 4(5):385–396.